A nocturnal breathing disorder – obstructive sleep apnea syndrome Trusted Source Obstructive sleep apnoea syndrome and its management Obstructive sleep apnoea (OSA) is a common disorder characterized by repetitive episodes of nocturnal breathing cessation due to upper airway collapse. OSA causes severe symptoms, such as excessive daytime somnolence, and is associated with a significant cardiovascular morbidity and mortality. Different treatment options are now available for an effective management of this disease. www.ncbi.nlm.nih.gov (OSAS) – robs many people, young and old, of long sleep and drive. One of the therapeutical options is the Continuous Positive Airway Pressure (CPAP) mask. But it doesn’t come without serious side effects, unlike the new CPAP alternatives available today.
Are you one of those patients who experience the side effects of the sleep apnea mask? Then you are not alone! Dry mouth, pressure points, and the like represent a great physical and psychological burden. This is why the acceptance of the CPAP mask continues to decline. It is no longer used regularly, the hoped-for effect does not materialize, and in the end, you discover you have achieved nothing for your health. It doesn’t have to be anymore. There are numerous treatment options nowadays in addition to the sleep apnea mask. In this article, we’ll show you an alternative way to treat your sleep apnea.
Around 40% of CPAP users suffer from dry mouth Trusted Source Common CPAP complaint: Dry mouth - Sleep Apnea If you’ve ever felt dry mouth when you take your CPAP mask off in the morning, you’re not alone. Roughly 40% of patients on CPAP therapy experience dry mouth. www.resmed.com , the most common side effect. In addition, many patients struggle with pressure points, pain, or allergies caused by the mask.
In addition, many find it difficult to fall asleep and/or sleep through the night with their technical equipment on. The mask creates anxiety. However, dry mouth and nose as well as other side effects mean that patients do not feel comfortable with this therapy. Finally, the technical background noise of the CPAP machine can also be an obstacle.

In addition to the classic sleep apnea mask, there are alternatives to the CPAP mask, both non-invasive and invasive for treating sleep apnea. Which procedure is suitable for you depends, among other things, on the severity of the sleep apnea and should be carried out individually after consulting your doctor.
Lifestyle changes are important and are the most affordable treatment alternatives to CPAP. You can treat mild cases of OSAS by changing some of your behaviors.

In addition to the usual places, they also attach to the throat and pharynx and narrow the airway. The apneas then arise. Therefore, a consistent diet and exercise program should be followed. After losing weight, it is crucial to maintain the new weight. Otherwise, there is a good chance that sleep apnea will recur.
Alcohol and nicotine should be avoided four hours before bedtime. Alcohol relaxes the muscles in our throats, which is why snoring and apneas can occur more frequently. Smoking is also a risk factor for developing OSAS. Nevertheless, because there is not yet enough medical evidence, a clear connection between smoking and alcohol is yet to be fully proven.
Medicines for sleep disorders and anxiety contain active ingredients which may relax the muscles. This can therefore lead to apnea. This includes in particular the substances benzodiazepine, barbiturates, and antihistamines.
Research has shown a decrease in the oxygen content in the blood in the long-term damages organs and metabolism and can lead to serious secondary diseases.
To date, however, there is a lack of broad, long-term studies investigating the effects of sedatives on people with sleep apnea.
In general, there are some rules of conduct for a healthy and restful sleep that you should follow. These include topics such as nutrition, exercise, sleeping environment, etc.
The sleeping position plays a significant role in the development of snoring. Sleeping in the supine position contributes to the fact that the back part of the tongue, the so-called base of the tongue, falls into the throat and narrows the airway due to the force of gravity. Basic tongue snoring and possibly apneas occur.
Position therapy can be a treatment option for OSAS caused by tongue arching. It includes products such as anti-snoring pillows, snoring vests, and snoring bandages.

Perhaps the best anti-snoring solution is the PureSleep Anti-Snoring Mouthpiece. These devices work against tongue base snoring by moving the lower jaw and at the same time the tongue base, which has grown there, by millimeters forward. This prevents the base of the tongue from falling back into the throat and blocking the airways.
At the moment, there are no suitable drugs for the treatment of sleep apnea whose effectiveness meets the criteria of evidence-based medicine. Treatments consist mainly of self-care, using lifestyle drugs that promote physical exercise and weight loss, palliative care, and surgery (palatoplasty, tonsillectomy, and adenoid removal).
If the non-invasive treatment methods are unsuccessful, the consideration remains to carry out an invasive, i.e. surgical, intervention. The aim of the operation is always to eliminate the cause of the apnea.
Depending on the severity of the sleep apnea and the nature of the upper respiratory tract, the procedure is carried out in the area of the nose, the palate, or in the area of the tongue or the base of the tongue.
Various methods exist accordingly. These include nose operations and jaw corrections for improving nasal breathing. Also, the tightening of your soft palate tissue, known as uvulopalatopharyngoplasty Trusted Source Uvulopalatopharyngoplasty (UPPP) Uvulopalatopharyngoplasty (UPPP) is surgery to open the upper airways by taking out extra tissue in the throat. It may be done to treat mild obstructive sleep apnea (OSA) or severe snoring. medlineplus.gov (UPPP), can be done when the small distance between the back of the pharynx and the soft palate is causing breathing pauses. The operation to remove the uvula (uvula flap) can be done.
In the field of tongue surgery, tongue base volume reduction is a solution. This method is now out of date. Instead, other therapy alternatives have opened up in recent years. These include implants installed below the base of the tongue as well as tongue pacemakers. This helps stimulate muscles located at your tongue base, preventing the tongue base from sinking back.
Respiratory supports can also be used. One of the most common and effective is the Breas Vivo 40 BiPAP ST, an invasive and non-invasive respiratory support that alerts caregivers of respiratory conditions.
We would like to briefly introduce two of these alternatives to CPAP treatment for sleep apnea.
This novel procedure is intended for patients with moderate to severe OSAS who cannot cope with the sleep apnea mask or for whom this conservative procedure does not work. A
clinical study
Trusted Source
Post-Approval Upper Airway Stimulation Predictors of Treatment Efficacy in the Adhere Registry
Upper airway stimulation (UAS) has been shown to reduce severity of obstructive sleep apnea (OSA). The aim of this registry was to identify predictors of UAS therapy response in an international multicenter registry. Patients who underwent UAS implantation in the US and Germany were enrolled in an observational registry.
erj.ersjournals.com
shows that the Inspire system was able to reduce the apnea phases by 68%.
Daytime sleepiness and snoring could also be alleviated. Another important prerequisite is that the patient is not severely overweight, which means that they have a good body mass index. A BMI of 30 kg/m² or higher is considered obese, according to the American Heart Organization.
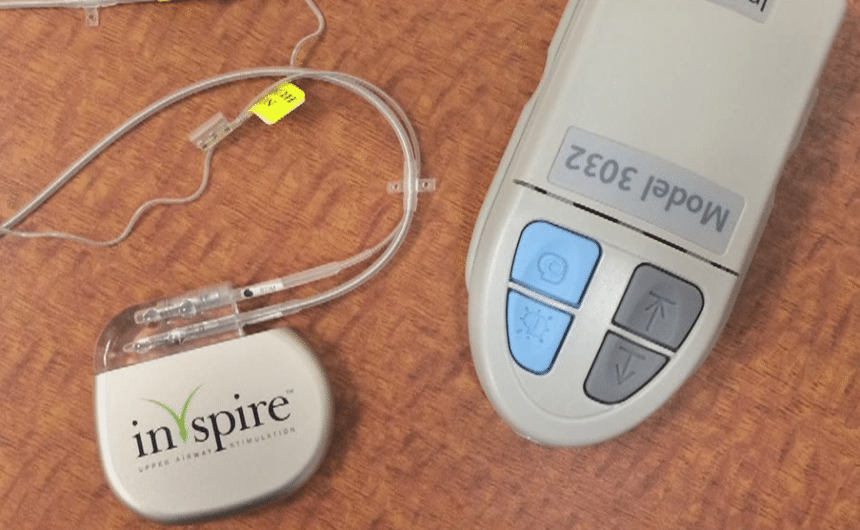
A typical Inspire system has three parts designed to be implanted into the skin. A chest sensor that measures your breathing rhythm while transmitting the data to a pacemaker-like generator will be inserted under your collarbone.
From there, one thin wire is connected to an electrode located on the muscles of the floor of the mouth under the chin.
If the chest sensor records any change in the rhythm of breathing, the pacemaker will send an electrical impulse to your pacemaker. In turn, this will prevent the collapse of the breathing area as it stimulates muscles on your mouth floor. This keeps the airways open while you sleep. A small remote activates the system before going to bed, and it is switched off again in the morning.
The Revent system is particularly suitable for OSAS patients in whom the airway obstruction is triggered by the base of the tongue slipping backward. The system is inserted through the skin into the floor of the mouth and tongue using a minimally invasive operation.
Functionality
These are one to four rod-shaped implants made of elastic silicone, at the end of which there is a loop. This is used for healing and fixation after implantation.
Before the operation, the implants are coated with a material that is broken down by the body a few weeks later. This causes contraction and thus prevents the base of the tongue from sliding backward. The elasticity of the implants does not affect normal tongue movements.
In addition to the health risks of the operation, success is ultimately not guaranteed. The higher the body mass index and the initial apnea-hypopnea index Trusted Source Apnea Hypopnea Index (AHI): Results, Treatment, and Related Testing AHI numbers (Alpha Hypopnea Index) are a method doctors use to classify the severity of sleep apnea in a person. Learn more about what these numbers mean for your sleep at WebMD. www.webmd.com (AHI), the lower the chances of success.
Not every sleep apnea has to be treated with CPAP therapy. After carefully preparing the findings and assessing the overall situation, the most sensible therapy option will be selected in a joint discussion between the patient and the doctor. In mild stages of the disease, possible CPAP alternatives range from dental splints to avoiding the supine position and other surgical measures.
Bodyweight has a central influence on the severity of obstructive sleep apnea. Weight reduction is therefore and desirable alternative. But it’s often not sufficient as an exclusive therapeutic measure and can usually neither be achieved easily nor quickly.
A direct treatment approach is offered by various alternatives that can be sufficient for mild disorders and can alleviate moderate-severe sleep apneas if CPAP is not tolerated or refused.